 Venous disease refers to all conditions caused by abnormal or diseased veins. It usually involves veins in the legs or arms, but can also involve veins in the chest, abdomen or pelvis. It generally includes blood clots—also called deep vein thrombosis or DVT—however, varicose veins, vein stenosis (narrowing), venous insufficiency (reflux of blood), pelvic congestion syndrome, spider veins, and compressive syndromes such as thoracic outlet syndrome are also common.
Venous disease refers to all conditions caused by abnormal or diseased veins. It usually involves veins in the legs or arms, but can also involve veins in the chest, abdomen or pelvis. It generally includes blood clots—also called deep vein thrombosis or DVT—however, varicose veins, vein stenosis (narrowing), venous insufficiency (reflux of blood), pelvic congestion syndrome, spider veins, and compressive syndromes such as thoracic outlet syndrome are also common.
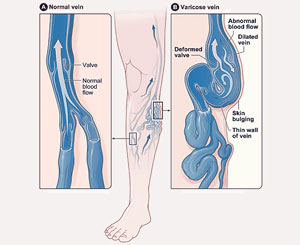
Veins have valves that keep blood flowing one-way back to the heart (from the rest of the body) each time the heart beats. When there is an interference in this one-way transport, venous insufficiency can occur.
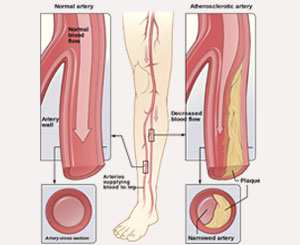
Venous insufficiency develops when vein valves break down and cause blood to flow backwards or away from the heart. This can lead to leg swelling and discoloration, heaviness, tiredness, and aching pain in the legs or pelvis. Venous insufficiency can also result in varicose veins, spider veins, pelvic congestion syndrome, and deep vein thrombosis or blood clots. Venous insufficiency affects as many as 30 million; however, only approximately 2 million receive treatment for their symptoms. Veins can also be narrowed or compressed, which may lead to blood clots and pain and swelling in the legs, arms, abdomen, and face, as well as conditions such as May-Thurner syndrome, Venous Thoracic Outlet Syndrome (Paget-Schroetter), and Nutcracker Syndrome.
Risk Factors
Certain risk factors that may lead to the development of venous disease include:
- Family history of vein problems or clotting disorders
- Obesity
- Pregnancy
- Prolonged standing or sitting
- Prior episodes of blood clot formation
- Trauma
- Illness
- Medications
Symptoms
Venous disease may cause no symptoms initially; however, if left untreated, can lead to swelling, pain, fatigue, heaviness, or ulcers on the legs that can make walking and performing everyday activities difficult. In some cases, there may also be brownish “freckled” discoloration of the skin, which is a result of blood pooling in the legs after refluxing the wrong way. Again, if left untreated, 20-25% of people with venous insufficiency will develop ulcers on their legs. In addition, bulging varicose veins can also form, which are not only painful and aesthetically unappealing, but may cause spontaneous bleeding as well.
Another form of serious venous disease is deep vein thrombosis (DVT), or clotting of the deeper veins. Blood clots may result from an injury, prolonged inactivity (such as an extended airplane ride or bed rest), certain medications (such as hormones and oral contraceptives), or a prior blood-clotting condition. DVT can cause pain, swelling, warmth, and redness in the legs, arms, abdomen, and pelvis. However, it can also be present without symptoms, which regularly occurs in over 2.5 million people and causes over 200,000 annual deaths from pulmonary embolism—a blood clot which travels to the lung. For this reason, it is critical that patients with DVT be promptly diagnosed and treated, so as to avoid dangerous complications.
Pelvic congestion syndrome (PCS) is another type of venous insufficiency involving the pelvic veins. In this circumstance, the veins that drain from the pelvis are not functioning properly and blood refluxes backwards to the pelvis. This is most common in women of childbearing age and often disappears after menopause. PCS has been recognized with increasing frequency as a cause of pelvic pain, which is aggravated by standing and may be associated with excessive menstrual bleeding, pain during intercourse, and bladder urgency. Varicose veins may also be seen in the genital area (varicoceles in men).
Venous thoracic outlet syndrome is caused by compression of the axillary and subclavian veins between the first rib and the clavicle (collar bone). This is usually in people who perform activities that require repetitive movement of their arms above their shoulders, such as hairdressers, painters, mechanics, and athletes (i.e. baseball pitchers, volleyball players, swimmers, and weightlifters). The compression of the vein leads to poor outflow of blood from the arm to the heart, which allows blood to pool in the arm. This can cause arm swelling, heaviness, fatigue, pain, and a bluish discoloration of arm or hand. It can also lead to a DVT or blood clot in the arm, which can be a life-threatening emergency.
Diagnosis
Superficial vein disease (varicose veins, spider veins) can be diagnosed through careful physical examination; however, superficial disease is usually a harbinger of deeper venous disease, such as venous insufficiency or DVT. Venous duplex ultrasound is the most effective way to test for deep venous disease in the legs, arms, or pelvis and in some cases, a venogram (an X-ray that uses intravenous dye to assess for blood clots, venous reflux, or vein stenosis) or CT scan may be necessary.
Treatment
The initial mainstay of treatment for all forms of venous insufficiency is graduated compression stockings and leg elevation. For patients with DVT, an anticoagulant medication or blood-thinner may be administered. For those with mild venous disease, such conservative therapies may be enough to control symptoms; however, if they are not successful, other procedures may be necessary to prevent serious complications should the following problems persist:
- Large, Painful Varicose Veins and Spider Veins
- Severe Venous Reflux
- Deep Vein Thrombosis refractory to medications
- Non-Healing Ulcer or Sores
- Vein Stenosis (narrowing)
- Venous Thoracic Outlet Syndrome
- Pelvic Congestio Syndrome
- May-Thurner Syndrome
Most treatments may be performed as an outpatient in the office and will involve injections or minimally-invasive catheter-based procedures that either seal off the diseased veins or removes them altogether. This prevents blood from refluxing backwards the wrong direction and pooling in the legs. Over time, the body will then turn the closed vein into scar tissue and nearby veins will take over the normal one-way blood flow back to the heart.
In addition, we have innovative endovascular techniques to remove blood clots from the veins through a tiny puncture in the skin, which allows blocked or narrowed veins to be opened through ballooning or stenting.
Patients with pelvic congestion syndrome may be treated with a variety or medications, including progesterone. If this fails, percutaneous embolization of the varices and diseased veins, with or without sclerotherapy, is an effective treatment.
For venous thoracic outlet syndrome, physical therapy exercises are used as a first-line of treatment in an effort to stretch out the space between the first rib and clavicle. If this is unsuccessful, then partial first rib resection—through a small incision—may be necessary.
Learn more about varicose veins Learn more about venous insufficiency